Viruses and Immunity: Who Prevails?
This is a translation of an article published on July 7, 2020 on the Russian-language science popularisation website biomolecula.ru
-

Venera Shakirova
Author and illustrator
-

Aigul Shakirova
Consultant, microbiologist
-

Natalia Chervochkina
Consultant, infectionist
-

Maria Dyakonova
Consultant, haematologist
-

Elena Belova
Editor
-

Andrey Panov
Editor
This work was published in the "Visually Explained" category of the "Bio/Mol/Text" Contest 2020/2021.
Amid the pandemic, people have shown more interest in scientific data as well as alternative medicine and various conspiracy theories. However, some of them do not even withstand the scrutiny of a highschool biology textbook. To protect ourselves from dangerous misconceptions, let's understand:
how viruses work;
why viruses need to enter the human body;
how the immune system responds to viruses;
how medicine can help the immune system if it cannot cope on its own.
*The article primarily focuses on the new coronavirus. – ed.
How the virus is structured
Human body consists of cells, in which proteins play a vital role. The cell nucleus contains DNA: you've probably seen pictures of these intertwined threads made up of variously coloured pieces.
The pieces are the same for everyone: humans, animals, plants, and viruses alike. It's the sequence of these DNA pieces that determines the characteristics of proteins in our bodies, thus influencing our appearance, organ function, and overall health.
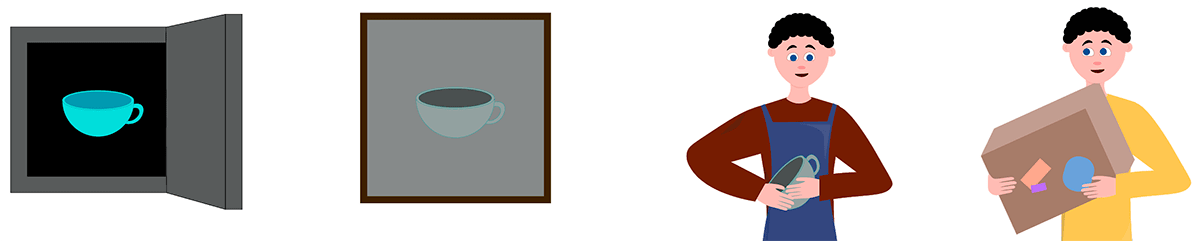
To understand how cells produce proteins, let's consider the following analogy.
Imagine you're making pottery. A super valuable model is kept in a safe, and you're not willing to take it out, not even to create a new copy. So, a potter makes a cast of the cup right inside the safe and gives the cast to the workers, who then produce a new cup based on the cast, receiving the necessary pieces of material from couriers.
At the cell nucleus, akin to a safe, DNA is stored. Using enzyme proteins, a copy of DNA is transcribed into messenger RNA (mRNA). mRNA then enters the ribosome, where the assembly of proteins begins. Meanwhile, transfer RNA (tRNA) delivers the fragments from which proteins are assembled.
* For further details, one can refer to the lectures of the cytology course by Igor Okhteyn, a biology teacher at the "Intellectual" lyceum and a methodologist of the Federal Children's Ecological and Biological Center of the Ministry of Education of Russia:
This is how protein production works not only in humans but also in many other living organisms.
They all adapt to the environment as best they can to survive and reproduce. Humans have also adapted, which was greatly aided by the brain. It has allowed them to invent adaptations for survival and transmit information to others. Through the exchange and accumulation of knowledge, humans can live very long lives because they have settled in sturdy buildings, invented numerous adaptations, and learned to cope with diseases [1].
In the past, humans faced threats from predators, weather disasters, a vast number of viruses, and bacteria from birth. Smallpox, plague, flu, malaria, rabies, encephalitis, tetanus — people died in hundreds and thousands from epidemics and even simple cuts. But thanks to medical advancements, we have learned to treat and prevent many of them [2], [3].
Nowadays, it may seem like these threats never existed at all. And if it turns out that they still exist, there is a strong desire to blame someone for their creation, as if they could not have arisen from nature themselves. But in fact, they could have.
Why does a virus need to enter the human body?
A virus differs from other living organisms because it does not feed, produce waste, or age (there is still debate on whether viruses should even be considered a form of life). However, like us, a virus reproduces and can die. A virus is like a flash drive: it has an outer shell with connector spikes, and inside, there is information (DNA or RNA).
With the help of its spikes, the virus attempts to enter the cell of the organism, much like a flash drive tries to connect to a computer. If successful, the virus penetrates inside, sheds its coat, and begins its subversion [4]. If the virus carries DNA inside, it secretly delivers it to the nucleus, interferes with the replication of this DNA, creates RNA, and so forth. If it carries RNA, it uses the cell's native RNA with its own [5].
In both cases, the cell produces proteins not for itself, but for the brand-new viruses.
When the cell has exhausted all its resources, it dies. From its remains, virus offspring jump out, which, with the help of their spikes, penetrate other cells, and the process repeats [6], [7].
How the immune system responds to viruses
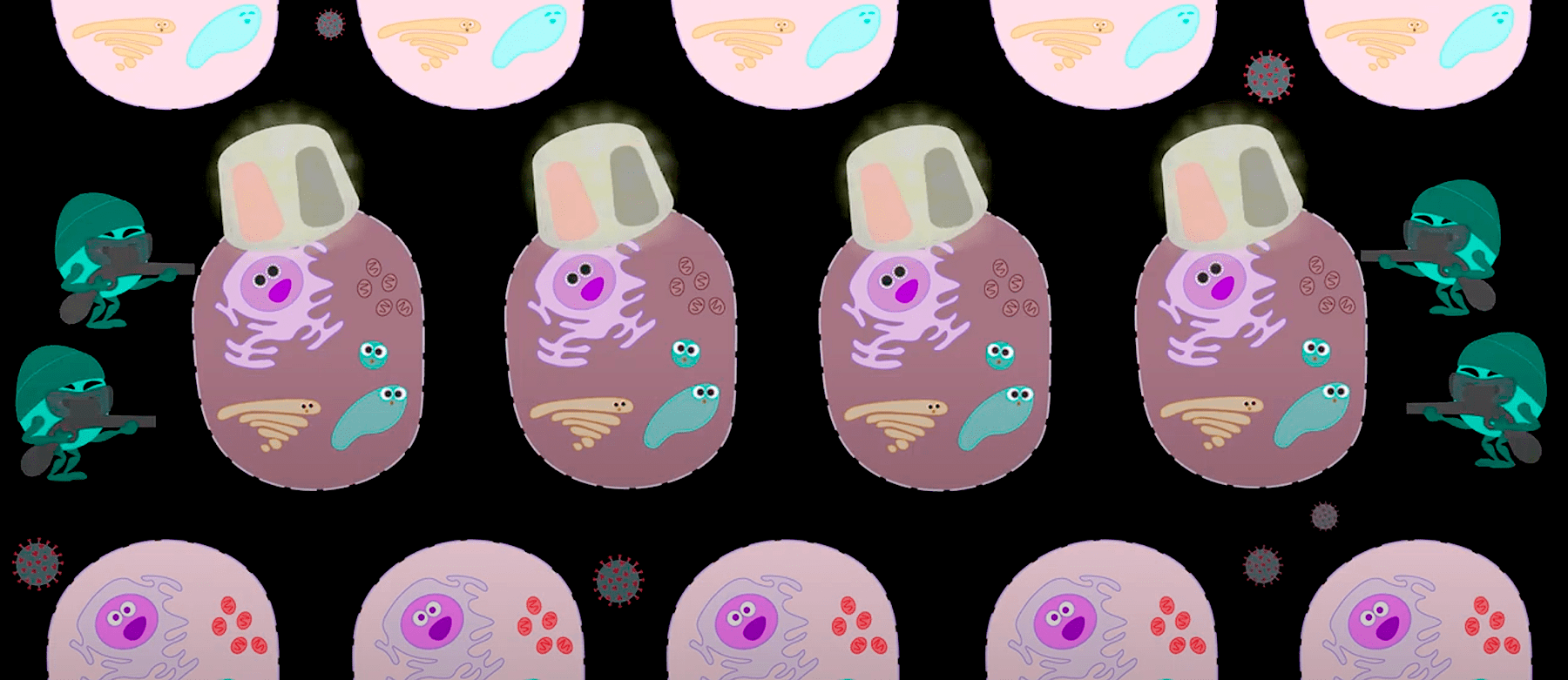
So, an intruder has invaded the body using our cells. The body must somehow respond. The immune system is precisely responsible for the body's ability to resist external threats. How does the immune response occur specifically to viruses? The key immune cells include phagocytes, B-lymphocytes, T-helper cells, and T-killer cells.
*The Latin letter B comes from the Latin term "bursa fabricii", an immune organ of birds where these cells were first discovered.
When a virus enters a cell, the cell displays a signal on the surface indicating that it is infected. Upon receiving this alarm signal, T-killers and phagocytes attempt to destroy the infected cells and viruses.
On their way, phagocytes capture the signal tag and pass it on to T-helper cells. These are courier cells that send the received material for examination to B-lymphocytes. They develop antibodies, special weapons against viruses and infected cells. Antibodies, like markers, attach to the infected cell, making it easier for T-killers to detect it quickly.
If the tag catches on a virus, another weapon responds to the signal - the complement system, similar to a grenade, which is triggered if two pieces of the grenade are connected together.
So, antibodies act as accelerators of the immune response, directing the attention of T-killers to infected cells and activating the complement system. This way, the body copes much faster and loses fewer healthy cells. Some B-lymphocytes, after studying the virus, instead of producing antibodies right away, remain armed with new knowledge in reserve in case of re-infection, transforming into memory cells. If the body encounters the virus again, it simply activates the memory cells. Thus, we get instant accurate shots from snipers and grenadiers [8], [9].
While all this commotion is happening, a person may become so unwell that hospitalisation or even intensive care becomes necessary. However, accumulated experience, technologies, and medicine must somehow assist such patients.
How can medicine assist the immune system if it fails to cope?
At what stage of the immune response can a person intervene? Let's start with the stage when the virus attempts to infiltrate the cell. The coronavirus has keys to mucous membranes: you can touch an infected object with your hands and transfer the infection to your body by touching your face. Carriers can sneeze or cough on you. Droplets of saliva are dispersed when you speak or laugh [10].
With hands, it's straightforward: you can wash away the top layer of skin fat, on which virus particles remain. But mucous membrane cells need to be somehow protected, for example, with a mask. However, it does not protect the eyes. Viruses, when they land on the mask, don't disappear — they accumulate there. It's important not to introduce them to your body system when adjusting or removing the mask. Homemade fabric masks may be useless if they have wide pores.
*It should be remembered that a mask only effectively prevents viruses from being released outwards, trapping liquid droplets on which viruses "attach." The mask provides extremely weak protection against viruses penetrating from the external environment into the interior. — ed.
The cardinal (and currently the best) method of protection is to go into quarantine. But in this case, it's not people’s health that suffers, but the economy.
Will prayers help? No, cells are structured the same in a clergyman, a grandmother, and a celebrity.
Will vodka help against the virus? No. When you drink alcohol, you don't disinfect the body, you only weaken it. This makes the work even harder for immune cells [12].
Garlic, ginger, and other wonders of folk medicine do not work as antiseptics [11]. To destroy a viral particle, a solution containing at least 60% alcohol is needed, for example, a special hand sanitizer. It's logical to use it to wipe hands, handrails, door handles, and mobile phones.
Suppose preventing the virus from entering the body failed. A melee ensues: phagocytes and T-killers are unable to cope, B-lymphocytes try to produce antibodies and memory cells, while the virus actively uses our cells. During this time, a person can become very ill.
Can we help B-lymphocytes? Yes, it's possible. Even before infection we can introduce a dead virus, a piece of the virus, or a virus-like particle so that B-lymphocytes can train and produce antibodies to the virus cells in advance. This method is called vaccination [13–16].
Another option is to introduce antibodies "from abroad." When B-lymphocytes fail, somebody else’s antibodies can be introduced into the body [17]. In some hospitals, plasma from the blood of those who have recovered is already being transfused – currently, this is an unofficial ("off-label") method [18].
The development of drugs takes years. It is necessary to find an active substance, a way to deliver it to cells, make it into a medication that will not spoil during storage and will not cause harm with side effects.
*The ClinicalTrials.gov website aggregates reports on clinical trials. — ed.
If a person becomes very ill, it is necessary to support their body so that they survive while the virus is being defeated. For this, people need hospital beds, ventilators, and doctors. But if the infection spreads rapidly, a lot of people require assistance simultaneously.
*Let us remember that invasive mechanical ventilation is traumatic and dangerous in itself: for example, because it can lead to the patient becoming infected with an additional nosocomial infection. - Ed.
To prevent people from dying in the absence of medical assistance, it is necessary to artificially slow down the rate of virus spread — by staying at home. The more people ignore the quarantine, the more people will not receive medical assistance, leading to more deaths [18].
If the body succeeds in fighting off the infection, it develops memory cells, so it will not be a carrier and will not infect other people. If the majority of people have memory cells, herd immunity will develop. Under such conditions, a person from the at-risk group is unlikely to encounter a carrier. When all the carriers recover, the virus will no longer occur among people.
Some countries are already lifting the quarantine. However, it is still unclear whether there is herd immunity and whether that will cause a new wave of infections. In the case of the coronavirus, it is still unknown how long memory cells live [19].
In Russia, 8,000 to 10,000 people are still getting sick every day. The pandemic might just be gaining momentum in your region. Therefore, any person on the street could be a carrier.
Here are some Russian and global statistics on the disease:
Official Russian data: стопкоронавирус.рф;
Overall global statistics from official sources: COVID-19 coronavirus pandemic.
It is within our power, if not to stop, then at least to slow down the pace so that people do not die without medical assistance.
What should people do in the fight against the virus?
Protect themselves by washing hands and using antiseptics? Look for a vaccine or medication? Wait until herd immunity develops? Or slow down social activity to prevent many people from getting sick at once? Right now, we are doing everything on this list.
Most countries in the world are following the WHO recommendations. The website of this organisation is available in Russian. There you can find comments on myths about the coronavirus and the official recommendations for both healthcare professionals and the general public. If someone offers you a miraculous cure for the disease, check if it has been endorsed by the WHO experts.
Literature:
[1] Harari, Y.N. Sapiens: A Brief History of Humankind. Moscow: "Sindbad", 2016. - 570 p.;
[2] Korotyaev, A.I. and Babichev, S.A. Medical Microbiology, Immunology, and Virology. St. Petersburg: "SpecLit", 2012. - 760 p.;
[3] History of Medicine. MGMU;
[4] Dömling, A., & Gao, L. (2020). Chemistry and Biology of SARS-CoV-2. Chem. 6, 1283-1295;
[5] Kalinin, V.L. Introduction to Molecular Virology. St. Petersburg: Publishing House of SPbSTU, 2002. - 301 p.;
[6] Astuti, I., & Ysrafil. (2020). Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2): An overview of viral structure and host response. Diabetes & Metabolic Syndrome: Clinical Research & Reviews. 14, 407-412;
[7] Pampel, J. (2020). SARS-CoV-2 life cycle: stages and inhibition targets. antibodies-online network;
[8] How the body reacts to viruses. (2020). Harvard Medical School;
[9] Klimpel, G.R. Immune defenses. In: Baron, S. Medical Microbiology (4th Edition). Galveston (TX): University of Texas Medical Branch at Galveston, 1996;
[10] COVID-19: answering questions, biomolecula.ru;
[11] WHO recommendations for the population regarding the spread of the new coronavirus (2019-nCoV): myths and misconceptions. (2020). WHO;
[12] Alcohol and COVID-19: what you need to know. (2020). WHO;
[13] Zverev, V.V. Vaccines and Vaccination: National Guidelines. Moscow: "GEOTAR-Media", 2014. - 640 p.;
[14] Vaccine development: what and how to simulate the disease?, biomolecula.ru;
[15] World before and after the invention of vaccines, biomolecula.ru;
[16] History of vaccination, biomolecula.ru;
[17] Saxena, S.K. Coronavirus Disease 2019 (COVID-19). Springer Singapore, 2020;
[18] Temporary recommendations of the Ministry of Health for the prevention, diagnosis, and treatment of the new coronavirus infection (COVID-19). (2020). Ministry of Health of the Russian Federation;
[19]Criteria for lifting isolation measures for patients with COVID-19. (2020). WHO.